
UCHealth doctors became the first in the western U.S. to perform a new “game-changing” surgery to help patients with thumb arthritis.
The new thumb arthritis surgery aims to give patients better function, faster recovery from surgery and reduced pain.
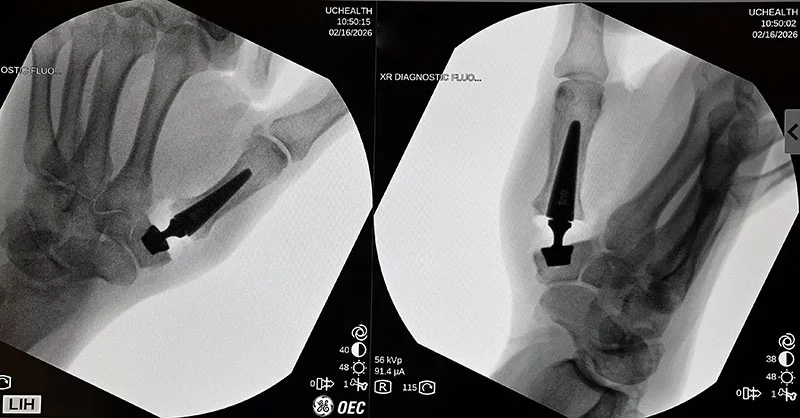
A team of University of Colorado Anschutz School of Medicine hand surgeons trained in Europe to learn the surgical technique and performed the new type of thumb surgery for the first time in the western U.S. at UCHealth University of Colorado Hospital on Feb. 16.
European hand surgeons have been doing this type of thumb arthritis surgery since 2018. Experts at the U.S. Food and Drug Administration (FDA) recently gave conditional approval for the prosthesis for U.S. patients.

The surgery on Monday went well. The patient was able to go home with only a soft dressing after her surgery and looks forward to having surgery on her other thumb in the spring.
“Everything went very smoothly,” said Dr. Fraser Leversedge, chief of hand surgery at University of Colorado Hospital. “The patient had a significant amount of arthritis.”
He said the team was able to remove the arthritic joint and implant the new prosthesis.
Dr. Louis Catalano, who also was part of the team that performed the first Colorado surgery on Monday, said the patient was doing well, and there were no surprises.
“The surgery went great thanks to all of our training and all of the studying we’ve been doing,” he said.
Thumb arthritis causes severe pain and grip weakness and is very common, affecting an estimated 7% of men and 15% of women — including as many as one-third of postmenopausal women.
Why surgeons are rethinking thumb arthritis surgery
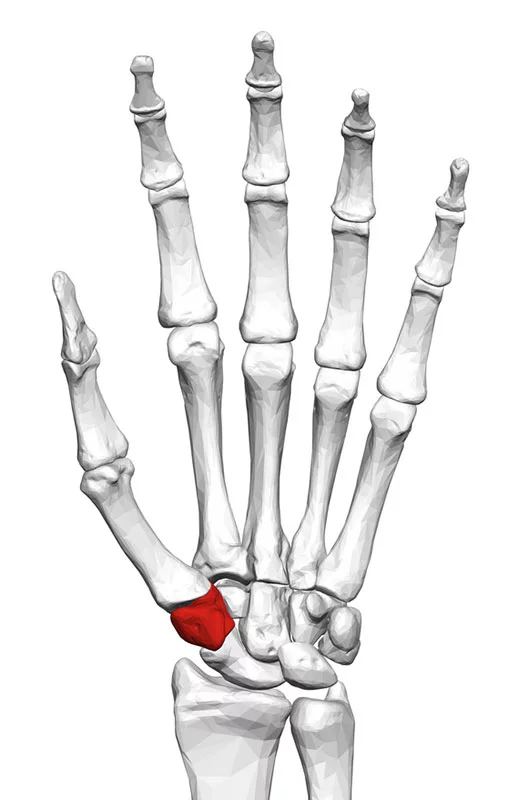
The trapezium is one of the eight carpal bones that help the wrist function. The trapezium doesn’t look like much. Averaging around a half inch in diameter and just under an inch long, it evokes an oversized molar that got lost on the way to the mouth.
The trapezium anchors the thumbs, and when it malfunctions, it can cause severe arthritic pain and associated grip weakness.
Until now, the go-to U.S. surgery to help with thumb arthritis — known as rhizarthrosis — typically results in significant pain for several weeks after the procedure. The standard surgery may lead to diminished thumb pinch strength and a slightly shorter thumb.
Thanks to a European innovation and months of local preparation and overseas training, the team from the Department of Orthopedics at University of Colorado Anschutz looks forward to bringing relief and the innovative new surgery to hundreds of patients in Colorado and the Rocky Mountain region. The doctors plan to train UCHealth colleagues elsewhere in Colorado and look forward to offering the new type of thumb arthritis surgery soon at multiple UCHealth facilities.
For now, the only other U.S. medical centers offering the new type of thumb arthritis surgery are in Texas, Illinois and on the East Coast.
A new type of thumb joint replacement surgery for thumb arthritis

The innovation takes the form of a Swiss-designed thumb prosthesis called the Touch CMC 1 Dual Mobility Trapeziometracarpal Prosthesis, which for sanity’s sake we’ll call the Touch CMC 1. It’s a ball joint that looks like “a hip replacement for a squirrel,” Catalano said.
Since European health officials approved the Touch CMC 1 in 2018, more than 150,000 European patients with thumb arthritis have had one implanted to replace a thumb-base joint, said Catalano, who is also an orthopedics professor at the University of Colorado Anschutz School of Medicine.
Based on years of use of the Touch CMC 1 in Europe, U.S. FDA officials granted premarket approval for the device in July 2025. That means the device can be sold, but final approval hinges on the maker proving its safety and effectiveness in a U.S. clinical trial.
The Colorado surgeons are one of just four U.S. groups participating in that clinical trial and are the first to offer the Touch CMC 1 to patients in the western U.S.
A major improvement over traditional thumb arthritis surgery
Catalano and fellow hand surgeons and University of Colorado Anschutz School of Medicine professors, Leversedge, Dr. Matthew Belton, and Dr. Mark Greyson, have been working to bring the Touch CMC 1 to Colorado since August. They trained in France, Belgium and Switzerland to learn the nuances of implanting the device.
The Colorado surgeons were uniformly impressed by how well the European patients did after the surgery. There’s less pain for a shorter amount of time, with likely better hand function in the end. In Europe, doctors do not need to give patients any opioid pain medications following the surgery. The UCHealth doctors hope their patients will similarly need fewer pain medications. And they expect their patients to recover much faster, too.
Catalano observed a woman in Europe who had had the surgery two weeks earlier. As she left the doctor’s office, she easily was able to twist the doorknob with her surgically repaired hand.
“In America, that’s a two-month process,” Catalano said.
Belton added, “Even the two-week patients were outperforming some of my patients at six months.”
Touch CMC 1 patients are known to leave the operating room with an Ace bandage around the hand. With the current U.S. surgery, called a thumb carpometacarpal (CMC) arthroplasty, patients are in a cast or a splint for six weeks.
Much less trauma with a thumb joint replacement
The improvements in pain, recovery time, and function boil down to the nature of the different surgeries.
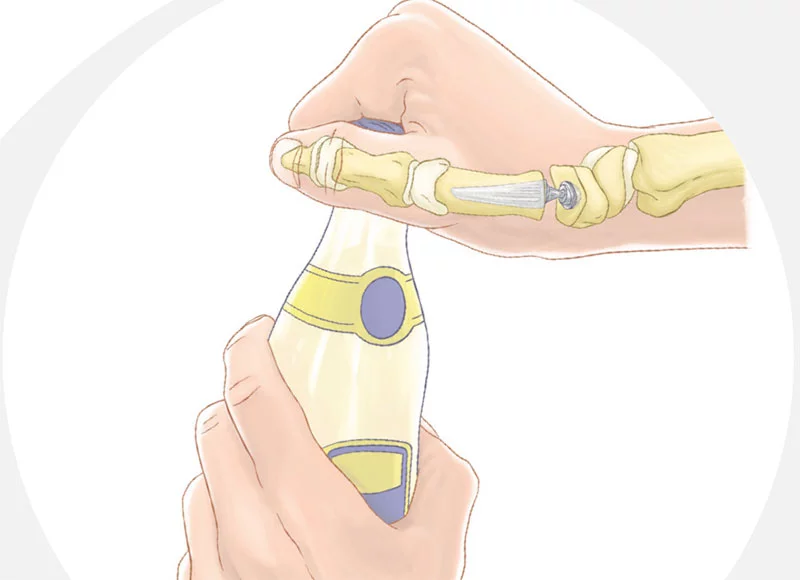
Traditional thumb CMC arthroplasty involves removing the trapezium bone. The surgeon then sutures together a bundle of wrist tendons to fill the space and help cushion the thumb’s biggest bone, the first metacarpal. In contrast, surgeons embed the Touch CMC 1 into the trapezium and the first metacarpal. That involves much less trauma and, by retaining the trapezium, there’s more underlying stability.
“It should be a lot less painful. It should make you feel like you have a normal thumb,” Catalano said. “With the patients we do now, even though the surgery works great, most patients don’t feel like they have a normal thumb because it collapses a little bit without the bone in place.”
About 50 UCHealth thumb arthritis patients who have exhausted nonsurgical options (anti-inflammatory medications, pain relievers, ice, splints/braces and injections, primarily) are lined up for the new procedure. They will, for now, get their thumb joint replacements at University of Colorado Hospital in Aurora, but the team is eager to provide the new surgery for as many patients as possible at other UCHealth facilities throughout Colorado soon.
“It’s hopefully going to be a game changer,” Catalano said.
