Vaccines are safe and effective. Get the facts.
Vaccines are an extremely safe and effective way to prevent disease by immunizing people to protect them from potentially deadly infectious diseases like measles, mumps and whooping cough.
Vaccines have prevented millions of deaths from infectious diseases.
The significant benefits of getting vaccinated
Historic victories over disease
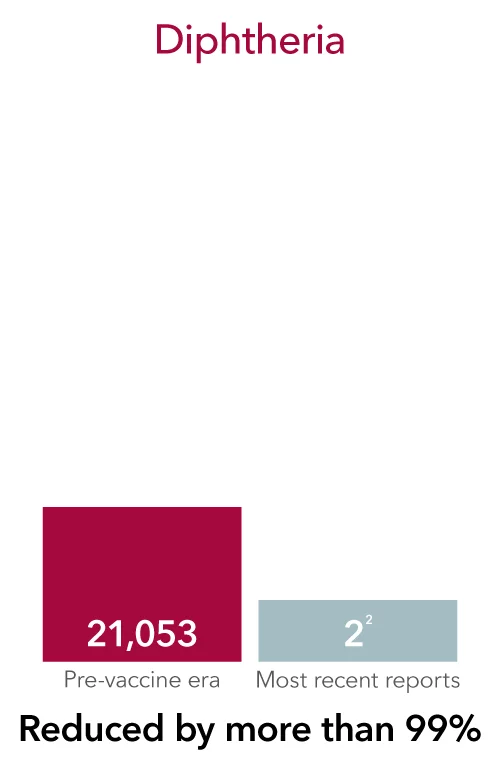
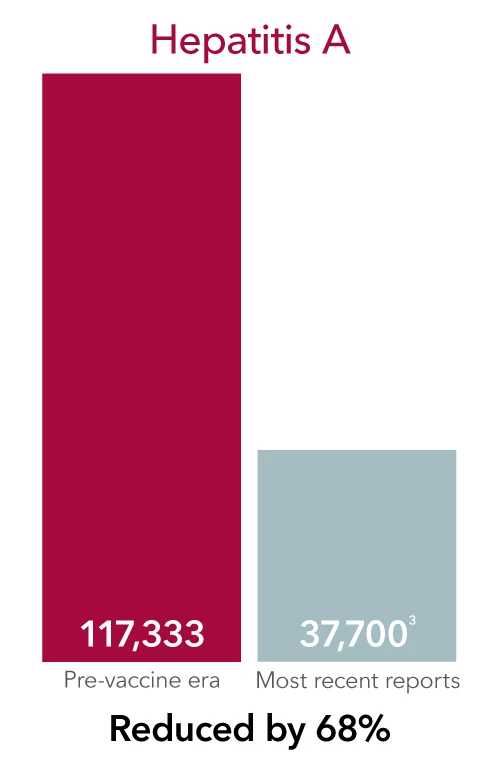
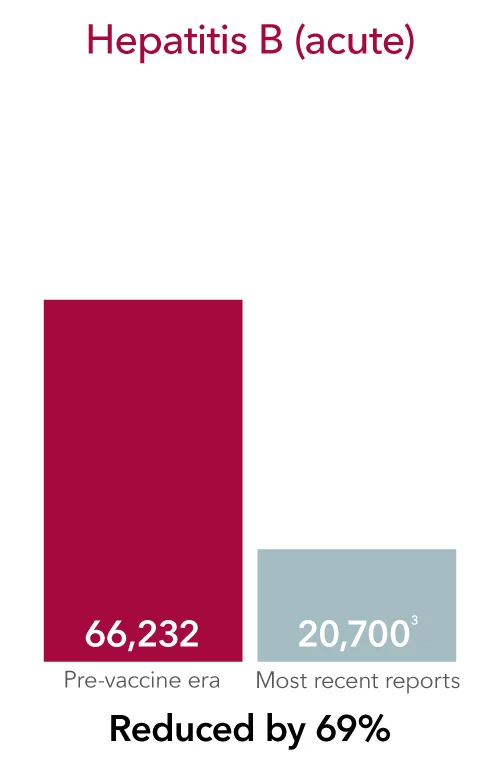
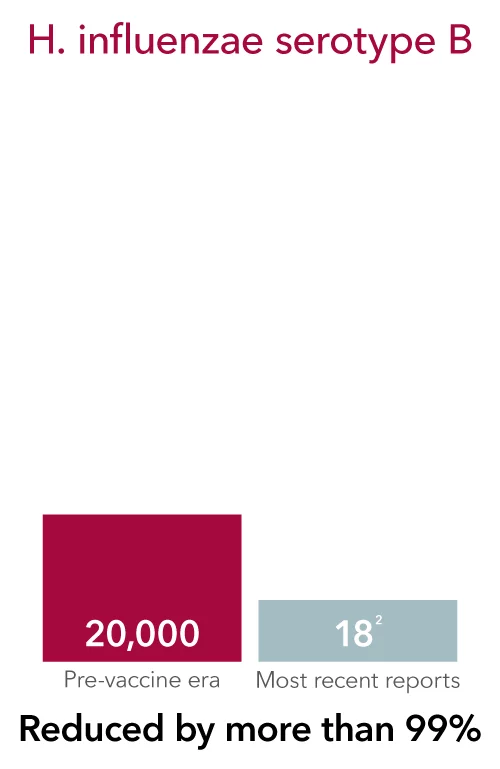
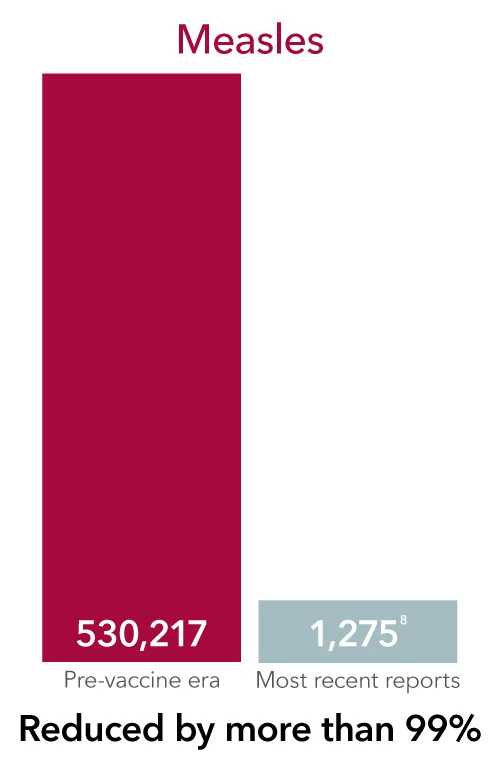
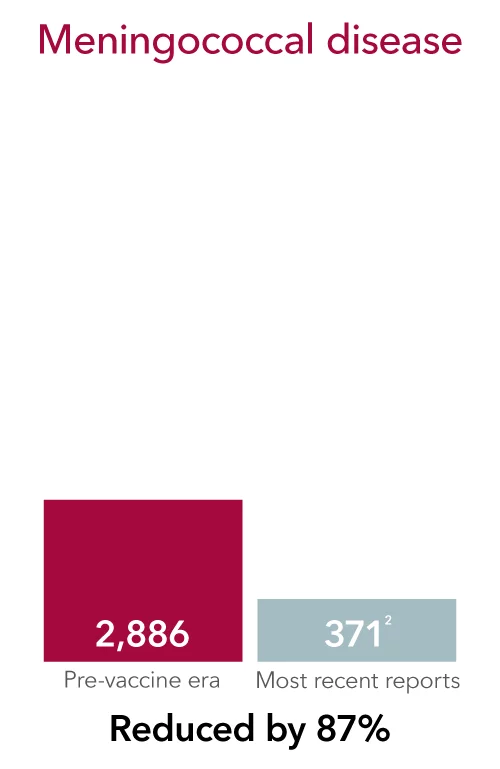
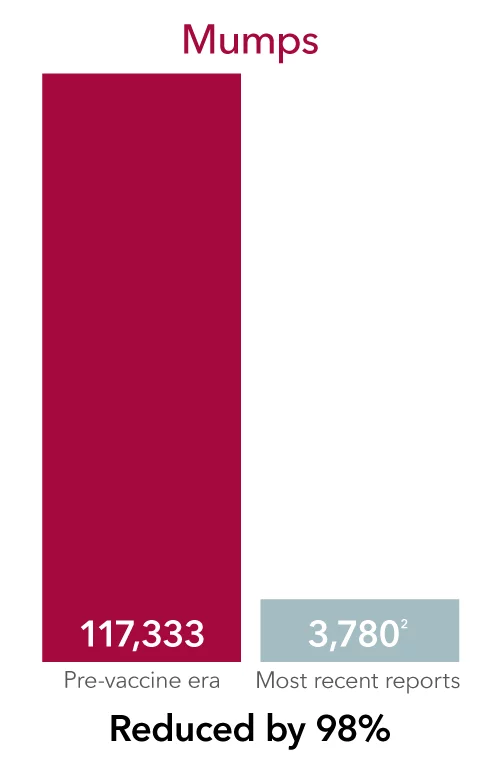
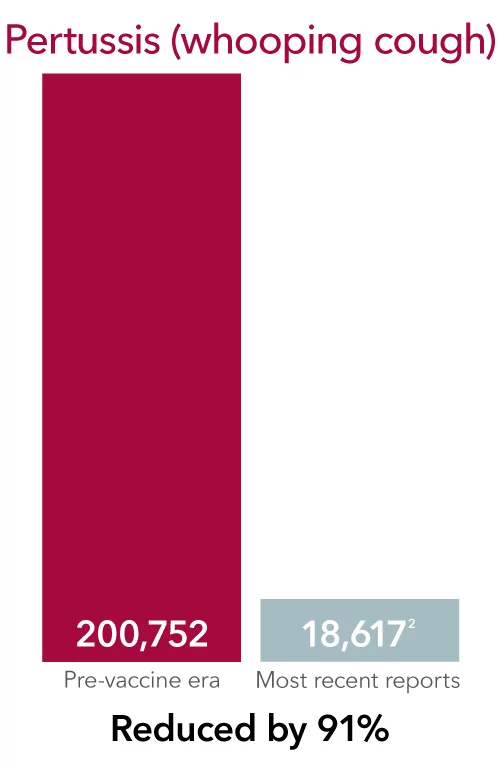
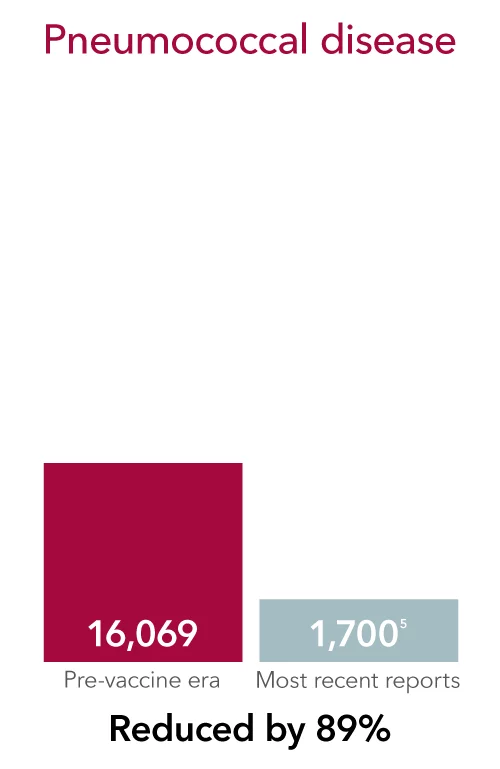
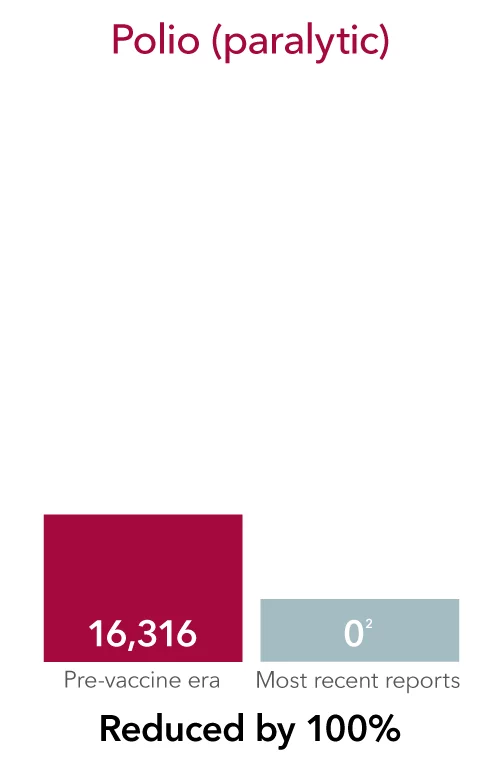
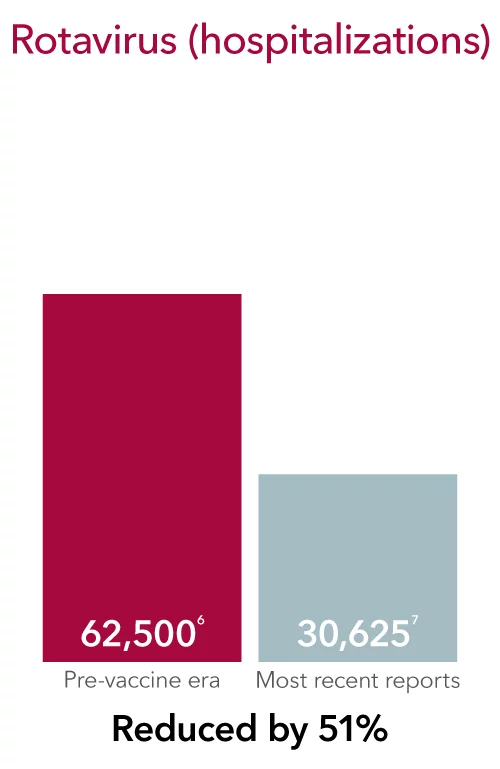
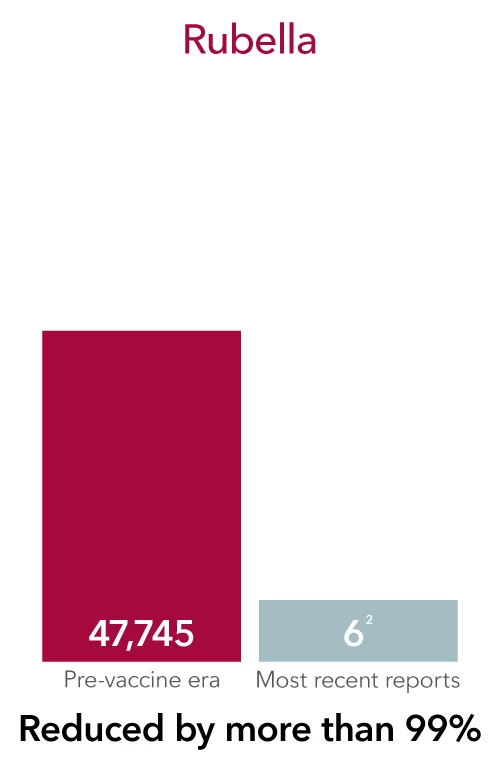
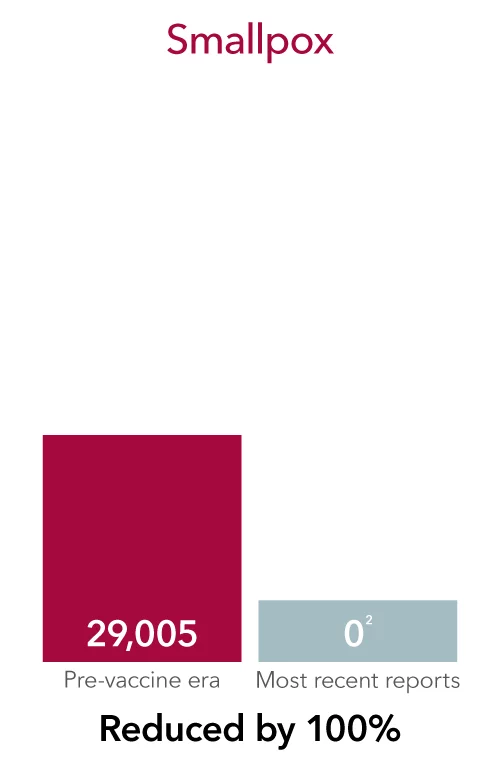
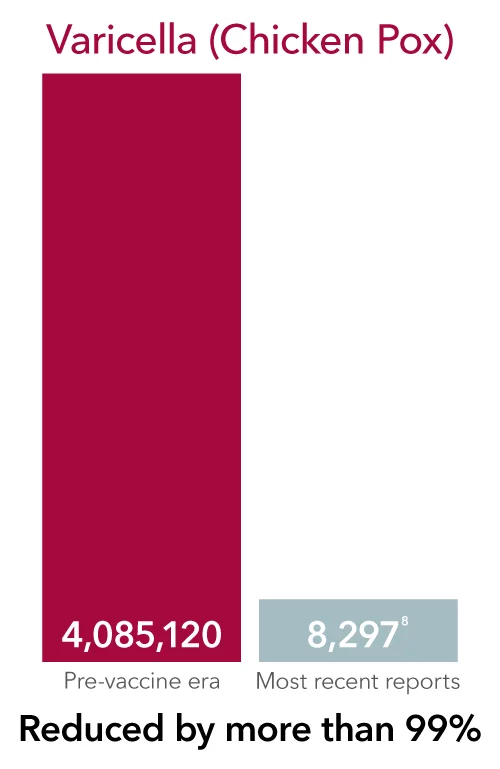
Vaccines have greatly reduced and even eradicated many infectious diseases that used to commonly harm—and even kill—people of all ages, all over the world.
Some of these diseases still exist, and you can get them if you aren’t vaccinated. In fact, thousands of adults in the U.S. become seriously ill and are hospitalized each year due to vaccine-preventable illnesses.
Safe and convenient
Vaccination is one of the most convenient and safest preventive care measures available. That’s why, for years, the U.S. Department of Health and Human Services has worked with federal and local partners to protect public health and prevent infectious diseases.
Visit your primary care provider for vaccination to help protect yourself, your family and your community.
Learn more about the most common vaccines
Flu (Influenza) vaccine
Everyone 6 months or older should get a flu vaccine, every season, especially people at higher risk of developing complications
People at risk
People at a higher risk for severe complications from influenza include:
- Adults 65 years and older
- Children younger than 2 years old
- People younger than 19 years old on long-term aspirin- or salicylate-containing medications
- Those with a weakened immune system due to disease (such as people with HIV or AIDS, or some cancers such as leukemia) or medications (such as those receiving chemotherapy or radiation treatment for cancer, or persons with chronic conditions requiring chronic corticosteroids or other drugs that suppress the immune system).
- People with certain disabilities—especially those who may have trouble with muscle function, lung function, or difficulty coughing, swallowing or clearing fluids from their airways.
- Pregnant women, including up to 2 weeks after the end of pregnancy
- Those who live in nursing homes and other long-term care facilities
- Certain racial and ethnic minority groups are at increased risk for hospitalization with flu, including non-Hispanic Black persons, Hispanic or Latino persons, and American Indian or Alaska Native persons.
Conditions that cause risk of complications
Certain medical conditions and disorders can increase your risk of complications:
- Asthma
- Chronic lung disease (such as chronic obstructive pulmonary disease [COPD] and cystic fibrosis)
- Neurologic and neurodevelopment conditions
- Blood disorders (such as sickle cell disease)
- Endocrine disorders (such as diabetes mellitus)
- Heart disease (such as congenital heart disease, congestive heart failure and coronary artery disease)
- Kidney disorders
- Liver disorders
- Metabolic disorders (such as inherited metabolic disorders and mitochondrial disorders)
- Body mass index (BMI) of 40 kg/m2 or higher/Obesity
- History of stroke
Since 2010 (except for 2020-2021 flu season), it is estimated that flu resulted in 120,000-170,000 hospitalizations and 6,300-52,000 deaths in the United States. Worldwide, flu causes 290,000-650,000 deaths annually.
What are some common myths about the flu vaccine?
COVID-19 vaccine
Who should be vaccinated against COVID-19?
Children 6 months – 23 months, children and teens age 2 – 18 years and with health conditions that increase the risk of severe COVID should be vaccinated with the Covid 2-dose vaccine. People living in long-term care facilities or other group settings, people who have never been vaccinated against COVID, or people who have household contacts who are at high risk for severe COVID should be vaccinated with the COVID 2-dose vaccine. Children 2-18 years without risk factors can get a single dose of the updated COVID vaccine. The updated COVID-19 vaccine or “booster” is also recommended at any point during pregnancy, when planning to become pregnant, in the postpartum period or when lactating. A COVID-19 vaccination is recommended for all adults, not just those at higher risk.
Conditions that do increase risk
Certain medical conditions and disorders can increase your risk of complications:
- Obesity
- Conditions that affect the immune system
- Sickle cell disease
- Heart disease or congenital heart conditions
- Lung disease (including asthma)
- Diabetes
- Neurodevelopmental disorders such as cerebral palsy
- Chronic kidney disease
- Complex medical conditions, including some that require breathing or feeding tubes, or home ventilators
Adults older than 65 are at highest risk of getting very sick from COVID-19. More than 81% of COVID-19 deaths occur in people over age 65. The number of deaths among people over age 65 is 97 times higher than among people ages 18-29 years. Your risk of severe illness from COVID-19 increases as the number of your underlying medical conditions increases. Some people are at higher risk of getting very sick or dying from COVID-19 because of where they live or work, or because they can’t get health care. This includes many people from racial and ethnic minority groups and people with disabilities.
What are some common myths about the COVID19 vaccine?
Respiratory Syncytial Virus (RSV) vaccine
Who should be vaccinated against RSV?
All adults ages 76 and older, and adults 50-75 who are at increased risk of severe RSV, should be vaccinated. Women who are pregnant during RSV season, or whose babies are due during RSV season, should get a single dose of the maternal RSV vaccine during weeks 32 through 36 of pregnancy – if those weeks fall between September and January.
The following conditions increase the risk of severe RSV
Certain medical conditions and disorders can increase your risk of complications:
- Chronic cardiovascular disease (e.g., heart failure, coronary artery disease or congenital heart disease [excluding isolated hypertension]).
- Chronic lung or respiratory disease (e.g., chronic obstructive pulmonary disease, emphysema, asthma, interstitial lung disease or cystic fibrosis).
- End-stage renal disease or dependence on hemodialysis or other renal replacement therapy.
- Diabetes mellitus complicated by chronic kidney disease, neuropathy, retinopathy or other end-organ damage, or requiring treatment with insulin or sodium-glucose cotransporter-2 (SGLT2) inhibitor.
- Neurologic or neuromuscular conditions causing impaired airway clearance or respiratory muscle weakness (e.g., post stroke dysphagia, amyotrophic lateral sclerosis or muscular dystrophy [excluding history of stroke without impaired airway clearance]).
- Chronic liver disease (e.g., cirrhosis).
- Chronic hematologic conditions (e.g., sickle cell disease or thalassemia).
- Severe obesity (body mass index ≥40 kg/m2).
- Moderate or severe immune compromise.
- Residence in a nursing home.
- Other chronic medical conditions or risk factors that a healthcare provider determines would increase the risk for severe disease due to viral respiratory infection (e.g., frailty, situations in which healthcare providers have concern for presence of undiagnosed chronic medical conditions, or residence in a remote or rural community where transportation of patients with severe RSV disease for escalation of medical care is challenging).
In 2024-2025, RSV was associated with 3.6 million-6.5 million RSV out-patient visits, 190,000-350,000 RSV hospitalizations, and 10,000-23,000 RSV deaths. Maternal RSV vaccine reduced the risk of the baby being hospitalized for RSV by 68% and risk of having a healthcare visit for RSV by 57% within 3 months after birth. In the same trial, the RSV vaccine reduced the risk of the baby being hospitalized for RSV by 57% and risk of having a healthcare visit for RSV by 51% within 6 months after birth.
What are some common myths about the RSV vaccine?
MMR: Measles, Mumps and Rubella (German measles) vaccine
Who should be vaccinated against MMR?
Infants should get their first dose between 12-15 months and their second dose at 4-6 years of age; all adults should have 2 documented doses of MMR or have documentation of titers that show protection.
Before the measles vaccination program started in 1963, an estimated 3-4 million people in the US got measles and 48,000 people were hospitalized with 500 deaths per year. There are on-going outbreaks of measles in the US, Canada, Mexico and the world, increasing risk of infection in unimmunized individuals. Mumps virus infection can cause inflammation in the testes or ovaries potentially leading to permanent infertility. It also can cause deafness, inflammation of the pancreas and inflammation of the brain. Rubella infection during pregnancy can cause a miscarriage or stillbirth. Congenital rubella syndrome which can cause growth delays, cataracts, deafness, congenital heart defects and learning disabilities occurs in up to 85% of infants born to people who had rubella in the first 12 weeks of pregnancy.
What are some common myths about the MMR vaccine?
Varicella (chickenpox) vaccine
Who should be vaccinated against chickenpox?
Infants should get their first dose between 12-15 months and their second dose between 4-6 years of age. People 13 years or older should get two doses 4-8 weeks apart without evidence of immunity (if more than 8 weeks since the first dose, the second dose may be given without restarting the series). The vaccine is also recommended for specific groups if they do not have evidence of immunity, including people with HIV infection, people with some degree of immunodeficiency, household contacts of immunocompromised people, postpartum and nursing mothers, and healthcare personnel.
“Chickenpox” used to infect 4 million people in the United States every year. More than 10,000 were hospitalized, and more than 100 died. A mild case can cause a child to miss school or daycare for a week or more.
What are some common myths about the chickenpox vaccine?
Herpes Zoster (Shingles) vaccine
Who should get the shingles vaccine?
Adults 50 years and older should receive 2 doses of vaccine separated by 2-6 months. Anyone 19 years or older with a weakened immune system should also receive the vaccine.
About 1 in every 3 people in the United States will have shingles in their lifetime and the risk of shingles increases with age. Shingles causes a painful rash and can be complicated by post-herpetic neuralgia (PHN), a long-term nerve pain which can be severe and debilitating. The pain occurs in the areas where the shingles rash was. PHN can last for months or years after the rash goes away.
What are some common myths about the shingles vaccine?
Hepatitis B vaccine
Who should get the Hepatitis B vaccine?
Children should get their first dose within 24 hours after birth. They can get their 2nd dose 4-8 weeks after 1st dose, and their 3rd dose approximately 6 months later and at least 4 months after the first dose. Children and adolescents age 7-18 years old can get their 1st dose at any time, their second dose 4 weeks later, and their 3rd dose 38 weeks later and at least 16 weeks after first dose. Age 19 years and older: 2, 3 or 4 doses depending on specific vaccine used and indications.
About 260 million people live with chronic hepatitis B. This means about 1 of every 32 people throughout the world are living with a chronic hepatitis B infection. Hepatitis B is 100 times more infectious than HIV. People most often get hepatitis B from contact with blood. Blood from a person infected with hepatitis B virus is heavily contaminated with the virus. The virus is present at such high levels that it can be spread by contact with quantities of blood too small to see. The virus can also survive on surfaces longer than most viruses — up to seven days. As a result, even casual contact with the blood of someone who is infected can cause infection. Casual contact can include sharing of washcloths, toothbrushes or razors. The virus can also spread among team members, particularly for contact sports where exposure to blood is more common. People have also been occasionally known to get hepatitis B from contaminated tattooing and medical equipment. People more likely to come into contact with the blood of infected individuals are at increased risk for hepatitis B. This includes healthcare workers, intravenous drug users and newborns of mothers infected with the virus. People can also be infected through sexual contact. The virus is present in semen and vaginal fluids.
What are some common myths about the Hepatitis B vaccine?
Human papillomavirus (HPV) vaccine
Who should get the HPV vaccine?
The minimum age for the HPV vaccine is 9 years. It is recommend to start between ages 9 and 12 years and to catch-up vaccination for all those not full vaccinated by age 18 years. If under 15 years, it is a 2 dose series 6-12 months apart. If over 15 years, it is a 3-dose series – dose 1, then dose 2: 1-2 months later and dose 3: 6 months after 1st dose. Recommended for adults 19-26 years and can be a consideration for adults 27-45 years but would recommend discussing with provider.
The HPV vaccine protects against infection from the human papilloma virus (HPV), which can lead to certain cancers and genital warts. It is a highly effective way to prevent more than 90% of cancers of the cervix, vagina, vulva, penis, anus and throat, as well as genital warts.
What are some common myths about the HPV vaccine?
You need vaccines throughout your life
You need to make sure your vaccinations are current because immunity can wear off as you age, and you are at risk for different diseases as an adult. The Centers for Disease Control and Prevention (CDC) recommends that all adults get immunizations to help them prevent getting and spreading serious diseases that could result in poor health, missed work, medical bills and not being able to care for family.
Your primary care provider will discuss with you the vaccine schedule for your age and condition, as well as for your children.
CDC recommendations for adults
According to the CDC, all adults:
- Need a seasonal flu (influenza) vaccine every year. Flu vaccine is especially important for people with chronic health conditions, pregnant women and older adults.
- Should get the Tdap vaccine once if they did not receive it as an adolescent to protect against pertussis (whooping cough), and then a Td (tetanus, diphtheria) booster shot every 10 years. In addition, women should get the Tdap vaccine each time they are pregnant, preferably at 27 through 36 weeks. Additionally, the CDC recommends tetanus vaccination for all babies and children, preteens, teens and adults.
Other vaccinations to consider
In addition, you may need other vaccines based on your age, health conditions, job, lifestyle or travel. The following diseases may be prevented by following the CDC guidelines for vaccines:
- Diphtheria. A serious disease caused by a toxin made by bacteria. It may damage the heart, lungs and nerves. It can be fatal.
- Haemophilus influenzae type b (Hib). A bacterial infection that leads to serious conditions such as meningitis, pneumonia and epiglottitis.
- Hepatitis A. A viral disease of the liver. You can get it by eating food or drinking water contaminated with feces, or you can get it by coming in contact with someone who has the infection.
- Meningococcal meningitis. A severe bacterial infection of the membranes that cover the brain and spinal cord (meninges) and can be life-threatening.
- Pneumococcal pneumonia. A serious lung infection caused by the bacteria Streptococcus pneumoniae.
- Polio. A highly infectious viral disease that affects the nervous system and may lead to permanent paralysis. Polio has almost been completely eradicated due to vaccines
- Rotavirus. A highly contagious virus that is the leading cause of severe diarrhea in children.
- Whooping cough (pertussis). A highly contagious respiratory disease that can lead to seizures, brain injury and death in young infants .
Side effects of vaccines
Vaccines are most often given through an injection, so the most common side effects are mild soreness, redness or swelling at the injection site, which go away in a few days.
Severe side effects are very rare. Your primary care provider will discuss possible side effects with you to help you decide what is best for you and your family.
The latest news in vaccines
References
Center for Disease Control and Prevention (CDC). Immunization Schedules – https://www.cdc.gov/vaccines/schedules/index.html
World Health Organization (WHO). Vaccines and immunization – https://www.who.int/health-topics/vaccines-and-immunization#tab=tab_1
Footnote:
- CDC. JAMA November 14, 2007; 298(18): 2155–63.
- CDC. National Notifiable Infectious Diseases and Conditions, United States: Annual Tables 2019. Accessed August 2, 2022.
- CDC. Viral Hepatitis Surveillance – United States, 2019. Published May 2021. Estimated total cases account for under-reporting.
- CDC. MMWR October 6, 1995; 43(53):1–98.
- CDC. Active Bacterial Core Surveillance (ABCs) Report; Emerging Infections Program Network Streptococcus pneumoniae, 2019.
- CDC. MMWR, February 6, 2009; 58(RR-2): 1–25.
- CDC. New Vaccine Surveillance Network, 2017 data (unpublished); U.S. rotavirus disease now has a biennial pattern.
- CDC. Varicella Program, 2017 data (unpublished)






