
Erica Brown loves Colorado. She hikes with her dogs, Ella and Sinatra, bikes with her husband, Matt Brown, and works out at the gym a few days a week.
She appears to be a picture of health. But six months ago, Erica experienced something no 32-year-old expects. She had a stroke.
In the early morning of Feb. 26, 2025, Erica woke with an intense migraine. She stumbled out of bed, then pinballed down her hallway.
Matt was getting ready to leave to go skiing, but he headed back inside to tell his wife of 10 years goodbye. Thankfully, he hadn’t left yet because it turned out Erica needed him and a big group of health professionals to save her life that morning.

When Matt went back inside, Erica was standing at the top of the stairs. She was looking down at him when he realized something was seriously wrong.
“She looked like she was going to pass out or faint, and I knew I needed to pull her away from the stairs,” Matt said.
Months earlier, Matt was getting his hair cut when he happened to have a random conversation about strokes. His barber’s partner, a young person like Erica, had suffered a stroke.
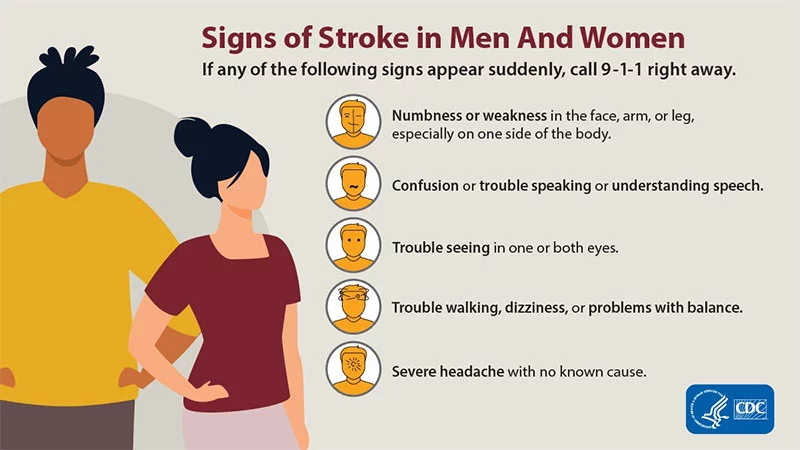
Erica’s confusion, her slurred speech and uncoordinated movements – these were all signs of a stroke.
After running up the stairs to keep his wife safe, Matt called 911 and followed the dispatcher’s instructions to perform several tests on Erica.
“They had phrases they wanted her to say. I had the phone on speaker, and I got the impression Erica didn’t believe that she was having a stroke,” he said. “I knew this was not normal. Her left side was not moving when she talked. I’m telling them, ‘This is not how she sounds.’ And within two to five minutes, we had first responders at the house.”
Paramedics rushed Erica to UCHealth Medical Center of the Rockies in Loveland, where a vascular interventional neurologist removed the clot that was causing Erica’s stroke. This life-saving intervention is called a thrombectomy,
Strokes can have devastating consequences, even in young, healthy people. They can cause speech and mobility deficits and, in some cases, death.
In Erica’s case, quick help from her husband, first responders and doctors led to a full recovery. Almost immediately after surgery, Erica regained her balance and speech and soon returned to biking and hiking.
Erica’s experience underscores how important it is for everyone to recognize common stroke symptoms and to know anyone can have a stroke — even a young adult.

The onset of stroke symptoms
Erica had been experiencing migraines about once a month for over a year. She always felt the sharp pain in a single spot — behind her right eye. But the pain she suffered that February morning was different.
“It was more intense that morning,” Erica said. “I got out of bed and fell, then got myself off the floor and walked headfirst into the bedroom door.”
Matt had gotten up early that morning to go skiing. He’d packed the car but headed back inside their split-level home to say goodbye when he heard the commotion. When he saw Erica at the top of the stairs, he thought it was strange she was up. It was around 6 a.m., and Erica’s not a morning person. But his thoughts quickly moved to panic as he saw her swaying. He bolted up the stairs, catching Erica in his arms before she could tumble down to him. He bearhugged his wife and laid her back down on the bed.

When Erica again tried to get out of bed without success, mumbling about needing the bathroom, Matt helped her down the hall. But while in the bathroom, her behavior became even more strange, and Erica’s reflection in the mirror told Matt all he needed to know – his wife must be having a stroke.
A conversation with his barber several months before had resurfaced. His barber’s partner, similar in age to Erica, had experienced a stroke while riding a motorcycle. The victim’s young age and overall good health left Matt with an impactful realization: anyone can have a stroke.
The number of strokes in people ages 18 to 45 has been growing at a faster rate nationally than any other age group in recent decades. Most recently, stroke prevalence increased nearly 15% between 2020 and 2022.
“People don’t want to think of a stroke at 32,” said Dr. Gautam Sachdeva, the vascular interventional neurologist who performed Erica’s thrombectomy that day. “They picture someone 70 or 80 with risk factors, but a stroke won’t spare you because you’re young.”
The importance of immediate response when it comes to a stroke
Within minutes of Matt’s 911 call, paramedics with Thompson Valley Emergency Medical Services and Loveland Fire Department were on the scene. Over the past two years, UCHealth has been educating emergency responders throughout northern Colorado and parts of Wyoming and Nebraska on recognizing the signs of stroke, specifically a “large stroke,” called an LVO or large vessel occlusion.
An LVO is a blockage in a major artery in the brain, which increases a patient’s risk of death by more than four times and reduces their chance of a good recovery by three times, according to one study.
Recognizing a large stroke before a patient arrives at the hospital speeds up treatment time.
“An ambulance can take you to care faster, but that’s not the only reason you should call 911,” Sachdeva said. “Emergency responders can recognize those signs and will take you to the right place that has the medical capabilities to take that blockage out.”
“They are alerting the stroke teams while still at the scene. That’s important because the earlier notice I get, the more likely we are to have the stroke team assembled by the time the patients get to us,” Sachdeva said.
That’s why it’s vital for patients to call 911 if they need emergency help. He said some people drive themselves to ERs and lose precious time.

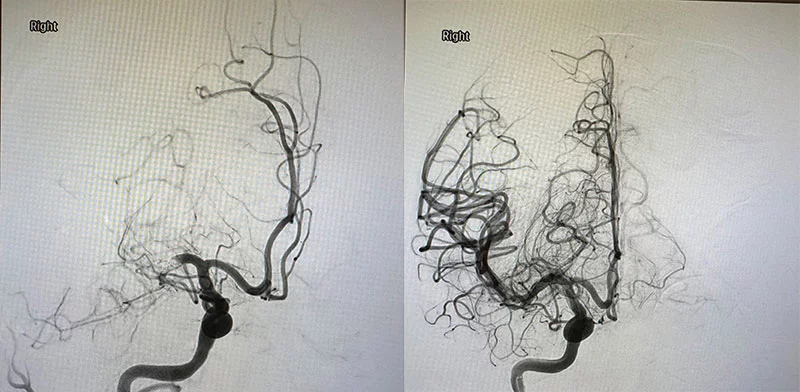
When Erica arrived at the hospital at 7:04 a.m., the stroke team had already been assembling for 10 minutes. A CT scan of Erica’s brain at 7:09 a.m. confirmed an LVO and determined the damage it had already caused.
“In Erica’s case, there was a large volume of brain tissue that could be saved,” Sachdeva said.

One of doctors’ first lines of treatment for a stroke is the clot-busting drug Intravenous Tenecteplase (IV TNK) administered through a vein. The drug breaks down the clot and restores blood flow.
Erica was not a candidate for this treatment because no one knew precisely when her stroke symptoms began, meaning they had no way of knowing if she was within the deadline for administering the medication.
“A lot of strokes happen in the middle of the night, and the person wakes, like Erica, with left-side weakness and difficult speech. We call it a “wake-up stroke,” Sachdeva said.
When a patient presents with LVO and is not a candidate for the clot-busting drug, “that’s where thrombectomy comes in,” he said.
Thrombectomy: An innovative medical intervention that diminishes the impact of a stroke
Sachdeva performs a thrombectomy by using a thin, flexible tube called a catheter that he inserts in an artery in the groin or through a patient’s arm. Guided by X-ray imaging, Sachdeva navigates the catheter to the clot in the brain. A device inserted through the catheter then removes the clot, either by pulling or suctioning it out.
Surgeons can perform thrombectomies on patients up to 24 hours after the onset of their symptoms, making the procedure an incredibly important tool in helping save brain tissue. But not all hospitals can offer the procedure. When a stroke patient arrives at a hospital that can’t perform a thrombectomy, doctors must transfer the patient to one that can. That process can take hours and tragically, can lead to more loss of viable brain tissue.
Sachdeva and the stroke team trained, educated and worked tirelessly over the past two years to establish a thrombectomy program at Medical Center of the Rockies. It is the only thrombectomy program between Denver, Colorado, and Casper, Wyoming.
“Every success along the way has been powered by collaboration — by EMS, ER, physicians, nurses, techs, radiology, ICU, support staff and countless others coming together with a shared purpose,” Sachdeva said. “This achievement is a true reflection of trust, coordination and commitment at every level.”
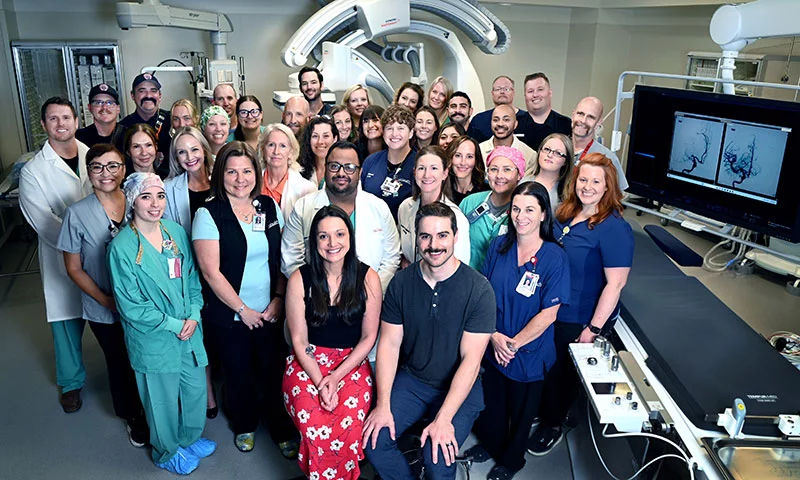
More than 100 stroke patients have benefited so far from the hospital’s thrombectomy experts.
“This isn’t just about a number. It’s about people: the patients whose lives were changed, the moments when every second mattered,” Sachdeva said.
Quick stroke response time and a stunning recovery
Just before 8 a.m. — less than two hours after Erica woke up that morning — Sachdeva was performing her thrombectomy. He and his team had fully restored blood flow to Erica’s brain by 8:32 a.m.
After the procedure, Sachdeva updated Matt. The procedure had gone well, and Erica was already talking.
Sachdeva explained that he was able to remove the entire clot, and tests revealed she was experiencing no deficits. She stayed at the hospital for two more days for monitoring before going home.
It was too soon to know exactly how well Erica would do over time, but Matt felt lucky and optimistic.
“It was a fortunate experience from an unfortunate experience,” Matt said.

Although young, stroke recovery is still challenging
Life after Erica’s stroke felt “strange,” the couple said. Because Erica didn’t have any noticeable deficits, Matt said friends who visited couldn’t believe she’d just been in an intensive care unit.
“It was like she’d just left to get her nails done,” he said.
Most people feel vulnerable after a major health crisis. For Erica, the experience hit her hard. She’d never imagined she could have a stroke, and her days in the hospital were all tough.
“It did feel like I had a stroke,” Erica said. “I was so exhausted.”
Less than a week after her stroke, she returned to her job as a data engineer, though she was less inclined to work late or sneak in an extra hour on the weekends, she said. Looking back, she said she wouldn’t recommend such a quick return to work.
“Take as much time as you need,” she said.
Although working in front of a computer screen didn’t bother her, she said she noticed impacts to her speech, such as forgetfulness, using the wrong words or jumbling words together. Over time, her speech has slowly been improving.
The stroke has taken a mental toll on the couple as well.
For weeks after the stroke, Matt couldn’t help but check on Erica frequently. He’d ask her to smile or have her raise her hand — some sign that she wasn’t having another stroke. Matt’s anxieties have eased somewhat, but he never leaves the house without telling Erica goodbye.

For Erica, being too far from home or far from emergency services is out of the question. She’ll still go on a 15-mile bike ride with Matt, but they kept it local.
“Staying around will be my plan for a while until I’m comfortable again,” she said.
The couple’s caution didn’t come from Erica’s doctors.
But the need to feel safe and close to help is “something that’s left” from the experience of having a stroke at such a young age.
“It’s hard psychologically,” she said. “My ego is wounded more than anything. I was doing the right things. I didn’t think it could happen to me, and it doesn’t seem real sometimes. But you accept it and keep moving forward.”

After Erica’s initial stroke treatment, doctors shifted to pinpointing the reason she had suffered a stroke so they could prevent a similar emergency in the future.
Unfortunately, they found no clear causes. Erica is now taking statin medications and baby aspirin daily. She had stopped taking estrogen-based birth control medication, which can elevate the risk of strokes in some young women, a few months before her stroke. But after her stroke, doctors advised her to stop taking her progestin-only oral contraception as well.
“I’m trying to live life normally. I’m getting back to the gym and over the fear that something could happen.”
Erica said she’s found solace in online support groups.
“I realize how fortunate I am that we caught it early,” she said.
