
Air Link’s registered flight nurses Duane Rorie and Leanna Harpman got the call: A 3-year-old female had been rescued by Poudre Fire Authority after being trapped in a closet fully immersed in flames. Poudre Valley Hospital Emergency Medical Services was transporting the patient to PVH, and air transport was needed to fly the child to Children’s Hospital Colorado in Aurora.
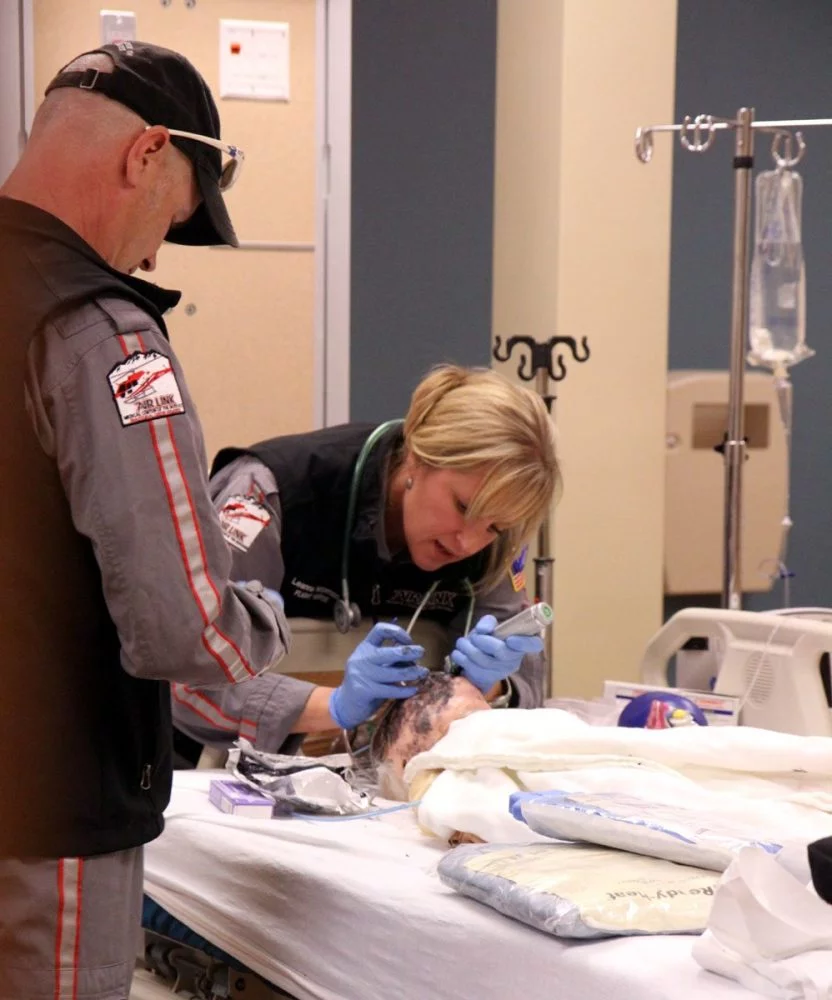
The two nurses — equipment bags in hand — rushed into a room to see their young burn patient on a hospital bed, exchanged information with the physician in the room and quickly got to work. As members of UCHealth Critical Care Transport Services, one of their duties is to safely transport patients between hospitals.
On this day, however, these flight nurses weren’t at PVH, and the little girl wasn’t real. They were in the UCHealth Clinical Education and Innovation Center’s simulation room, working to save a high-fidelity simulation mannequin. For Rorie and Harpman, though, the situation was “real’’ and they concentrated on learning valuable insight and honing their skills.
“This is a high-risk, low-frequency patient, but one that the critical care team could see later today or tomorrow,” said Nate Hinze, a flight RN for Air Link at Medical Center of the Rockies and a trained simulation educator. “So our goal is to make this as real as possible.”
And it is.

CEIC has six high-fidelity simulators ranging in age from newborn to adult. These “mannequins” have realistic abilities. They are able to open their eyes and breathe, emit throat and lung sounds and talk and cry.
“Instead of reading a paper that says, ‘The patient isn’t breathing well; what do you do next?’, the nurses have to use their assessment skills and critical thinking just as if this was a real patient,” said Laura Wining, coordinator of education programs for UCHealth’s simulation lab at the CEIC.
Also important to this type of training is that it takes place in a room similar to a hospital room, with realistic props that nurses would see in a real situation. Rorie and Harpman’s patient wore burned clothing and theater makeup to help portray realistic wounds.
“This helps them (the nurses) be more immersed and really feel like it’s a real patient they are caring for,” Wining said.
Just then, as Harpman struggled to get a breathing tube into the child’s throat, she leaned down and said, “Sorry, baby,” to the child.
“Those are the cues we look for to see if they are immersed — that’s an actual function that any caregiver would do in a real crisis,” Wining said, referring to Harpman’s action. “When we see that, we know we are accomplishing our goal: making it as realistic to a patient scenario as possible so the participant can take forward that knowledge they learned to help future patients.”
Realism is the key piece in helping providers learn — a research-supported fact, she added.
To enhance realism, clinical educators Hinze and flight RN Ryan Bushmaker, control the scenario from behind one-way glass. They can hear what is going on in the simulation room, control the mannequin, and even call and answer the phone, acting as physicians or medical experts.
“Hospital-based simulation labs are still a growing education area,” Wining said. “In the academic setting simulation has proven its worth within nursing education as well…it’s amazing what the training has allowed us to do.”
The simulation lab is conducive to group training. For example, as many as 15 participants from all areas of medicine have participated in the care of a critically ill simulation mannequin before at the center.

Bushmaker, who only a few days before the simulation training had a pediatric burn patient in his care, said the training also helps the whole team identify areas for process improvements or protocol changes.
“The participants report that they appreciate the safe learning environment and getting questions answered that they haven’t been able to ask in prior situations,” Wining said. “And we know that we’ve improved patient outcomes by increasing knowledge, team communication and through routine monitoring of quality indicators.”
