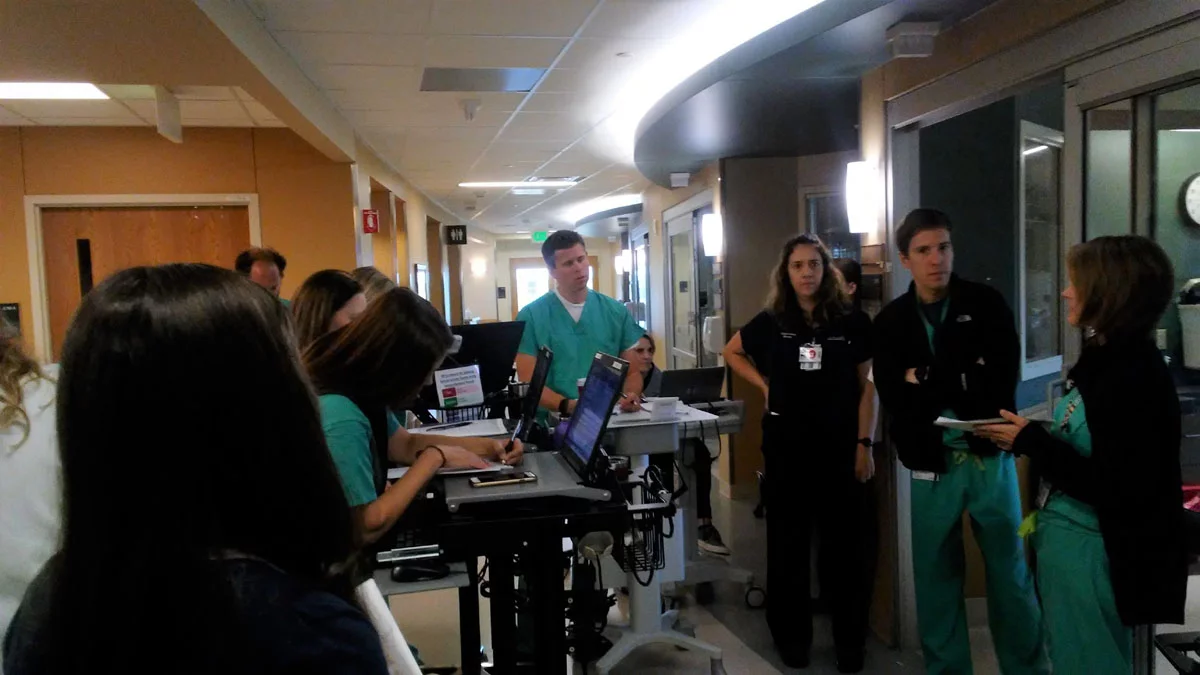
It’s a Thursday morning on the Surgical Trauma Intensive Care Unit (STICU) at UCHealth University of Colorado Hospital. Physicians, advanced practice providers, nurses, dieticians, care managers, pharmacists and others gather around one of three unit workstations, tapping on laptops, discussing cases, scribbling notes, and cracking a joke or two.
Shortly before 8 a.m., Dr. Jason Brainard, an anesthesiologist and co-medical director of the STICU, assembles a small brigade of providers and calls for their attention. They set off down one hall of the 24-bed unit, pushing computers on wheels, thumbing cellphone screens and quietly conferring as they start the daily task of morning patient rounds.
At each room, the team stops and a resident or advanced practice provider summarizes the facts of the patient’s illness or injury and the care that is being provided. Brainard asks questions and initiates discussions with the entire team about a litany of concerns – pain levels, oxygen needs, diet, drains, medications, mobility, and blood thinners, blood sugars, blood pressure, and blood gases – while the busy unit hums around them. The team summarizes the case, finalizes a plan of care for the day, then trundles off to the next room.
There is nothing unusual with their routine, save for one addition. At several rooms Brainard and company visit, the team grows by at least one member: a family member, sometimes simply listening, other times interjecting questions about the care. Depending on their condition, patients may join in as well.
Open invitation
Patients and family members participating in rounds is now the standard in the STICU, thanks in large part to the efforts of two critical-care nurses, Alicia Morris and Farrell Thayer, who spearheaded the initiative as members of UCH’s graduate nurse residency program in October 2016. After completing a literature review of patient and family participation in ICU rounds, Morris and Thayer found the practice had been studied relatively rarely, even though the American College of Critical Care Medicine guidelines recommend it.

The two nurses worked with unit pharmacist Bonnie Boller to audit rounds on the STICU for two months and found that a family member was present and actively listening only 28 percent of the time (although Morris noted that in some cases, patients had no family members or loved ones to represent them during rounds).
Based on their data collection and their own experience, Morris and Thayer concluded that formally involving families in patient rounds could greatly benefit patients, family members and providers.
“We thought rounds are an easy way to introduce the team to the family and the family to the team,” Morris said. “The family can see the team rounding, breaking down the plan of care and discussing how things are changing with the patient. Family members who are prepped and experiencing the plan of care can become strong representatives for themselves and for the patient.”
Personal involvement
Elyse Bueno, nurse manager of the STICU, encouraged Morris and Thayer to implement the rounds. As a member of UCH’s Patient Experience Action Team, Bueno noted that she’d seen the need for the hospital to bolster its communication with patients and family members, many of whom struggle with both physical and emotional trauma.
“The complexity of care in many cases is incredible,” Bueno said. “We all need to look for ways to connect with patients and develop a plan of care together.”
In the STICU and other ICUs, for example, a key question is what patients need to do to move on to the next level of care, she added. “That’s an important step in recovery,” Bueno said. “Rounds are pivotal for the entire interprofessional team to build on the plan of care, and it makes sense to pull patients and family members into the discussion. They like participating and having a role.”

The plan roll-out included educating STICU nurses – all of whom participate in rounds – about the potential benefits of inviting patients and family members into rounds and getting buy-in from physicians and advanced practice providers, Morris said. She and Thayer also produced a pamphlet explaining the rounding policy to patients. The trifold includes space for written questions nurses can ask other care team members on the patient’s behalf. With those in hand, providers can and do drop by patients’ rooms later in the day – rounds run from 8 a.m. to noon – to offer additional information and explanation.
Brainard said the patient rounds are less wholesale change than a shift in emphasis on delivering care. “We never had a policy for not including patients and family members,” he said. “But now we have formalized and advertised the introduction of family members joining us each morning for rounds.”
Benefits outweigh challenges
Some providers expressed concerns that adding other voices to the rounding mix could decrease efficiency, a valid question on a unit with many complex cases, Brainard said.

“Like every unit in the hospital, we’ve experienced tremendous growth, and efficiency is important to us,” he said. But he added that in most cases, the extra three to five minutes the team might spend answering questions pays off over the course of the day because patients and their caregivers are better informed, have fewer concerns, and ultimately have a better patient experience.
“More importantly, the rounds are very constructive in building positive relationships with the care team, improving family members’ education, and developing shared clinical decision-making. All together, we believe this communication improves the care we provide to our patients,” Brainard said.
The STICU will undoubtedly get high marks from Richie Davidowski and parents Kelly and Richard, who were on the unit that recent Thursday morning. Richie, 29, had received a new liver to replace the original organ damaged by Budd-Chiari syndrome, a congenital problem that blocks the veins that drain the liver. Richie, a service manager for a construction company in Fort Collins, said he fell seriously ill two years ago. He was admitted to UCHealth Poudre Valley Hospital, where he was diagnosed and placed on the liver transplant waiting list at UCH.
Richie was weak from prolonged critical illness and recovery from the liver transplant and subsequent surgeries, but Kelly and Richard, who had flown in from Danbury, Connecticut, were upbeat. “We’re ecstatic,” Kelly said. “He’s much better than we expected.”
Minutes before, she’d stood at the door of Richie’s room, listening while Brainard and his team ran through his case. They discussed improving his respiratory status, advancing his diet, getting him up to walk, and managing his anticoagulant medications to prevent further clotting.
“Richie has progressed extremely well,” Brainard said.
“We appreciate it,” Kelly said of the rounding after the team left. “It’s very informative and we’re not getting secondhand information. They come in and explain things in simple terms – what they’re doing, what they’re giving him and why. We’ve felt embraced from the moment we walked into this hospital.”
That response is what Morris and Thayer hoped for when they launched the rounding project.
“Our patients have been through traumatizing experiences,” she said. “The better we communicate with them, the better they will be able to advocate for themselves, and the better off they will be.”
