
Olivia Thornton is a wife and mother of three young boys, ages 4, 6 and 7, but she barely gets to spend time with her husband or children these days.
It’s still pitch black and cold outside when Olivia slips out of bed and joins a daily call at 4:30 a.m. with other nursing leaders to learn how tough the day ahead could be. Then she quietly slips out of the house long before the boys wake up and wander out with tousled hair looking for breakfast and their mom.
Olivia arrives by about 6 a.m. at UCHealth University of Colorado Hospital where she cares for patients and helps manage one of the COVID-19 ICUs. It was the hospital’s first ICU to be designated in the spring specifically for patients suffering from what was then a mysterious new coronavirus.
Since then, Olivia’s unit has never stopped caring for COVID-19 patients.
The life of a pandemic nurse
Throughout the summer and early fall, even when COVID-19 hospitalizations were at their lowest levels in Colorado, Olivia and her team still were caring for critically ill patients around the clock. Now, this COVID-19 ICU and many others are filling up fast again.
The pandemic nurses’ weary eyes show above their masks, but they remain dedicated to their mission: giving excellent, loving care to people who cannot have their own loved ones by their sides.
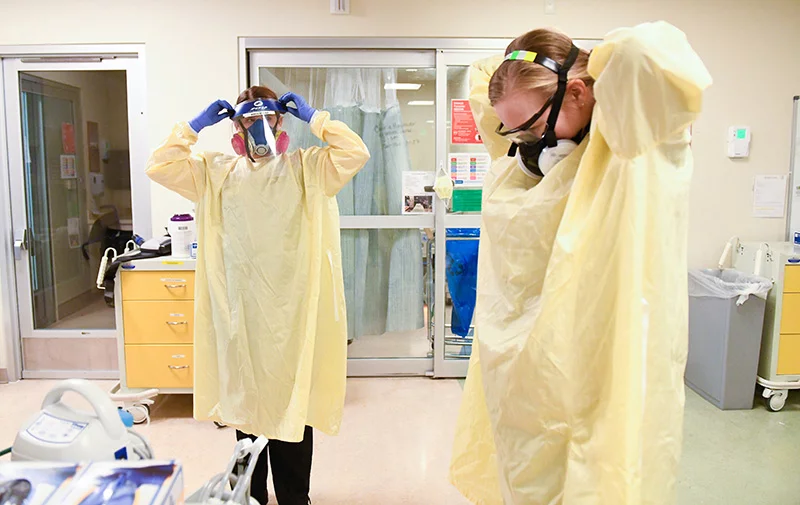
When Olivia goes into a patient’s room, she must suit up in full protective gear: a yellow plastic gown, blue gloves, a mask and a face shield over that. All the gear is cumbersome and hot to wear, but it keeps her safe. She is not afraid.
As Olivia does her work, she takes time to connect with each human being in her care.
“You just hold someone’s hand and let them know, ‘Hey, you’re doing great. It’s OK. We’re here for you.’ It’s heartbreaking watching these people who are here all alone.” (Watch this video to see how a sense of teamwork among care givers has never been stronger.)

The pandemic in the United States: better survival rates now
There have been many happy stories of people who have lived. And survival rates are much better now than they were in the spring. Nurses and doctors have learned how to better care for patients, while they also have some new therapies and medications. Patients are spending fewer days in the ICUs and fewer patients are dying from COVID-19 now.
But, there have been crushing losses too. Olivia spent hours talking with the wife of one patient. The couple was supposed to be moving into a new home together. Instead, the wife had to make the devastating decision to let her husband go and receive comfort care in his final hours. The woman’s husband and the couple’s dreams died.
“There are these heartbreaking stories of families and plans they have made,” Olivia said. “The hardest thing is that these families can’t be together.”
Along with being emotionally exhausting, the work is taxing too.
Health care workers in the time of COVID-19: Long days, tough jobs for pandemic nurses
Clinical nurses have to suit up in personal protective equipment about 20 times during each 12-hour shift. Depending on all of the tasks they need to do for their patients, they might spend 90 minutes at a time in full gear before coming out of a patient’s room, wiping down their masks, changing out of their protective gear and getting ready to start the process all over again.
“It’s very hot. It’s hard to breathe. But, after a while, it becomes second nature. We are very, very good about making sure that everyone is being careful and doing exactly what they need to do to stay safe,” Olivia said.

Along with one of the COVID ICUs, Olivia also helps manage a medical ICU that does not yet have COVID patients. She also helps manage the wound care team and clinical resource nurses. She credits all of her nurses with doing extraordinary work. They, in turn, say they couldn’t do their jobs without Olivia’s leadership and dedication.
Olivia tries to leave work by 6 p.m., but on a recent night, she wasn’t home until 9 p.m. The boys were already asleep. Another day had passed and she hadn’t been able to see them at all, even for breakfast or bedtime stories.
While she and many other medical providers have sacrificed seeing their own loved ones, she and others are calling on people to please stay home so they can protect one another and so that fewer people will need to go to hospitals.
“For us, that’s the biggest struggle. We realize how hard it is not to be able to go see your friends. But, it could kill you. I know people think that there’s a low percentage chance that anything bad will happen. But some will die.
“You truly can’t understand what some of these patients go through,” she said. “You just don’t know what it’s going to do to you.”
She has seen people of all ages who have been gravely ill.
“You think that this mostly affects older, overweight, hypertensive people, then you get a fit 20-year-old boy who is very, very ill,” she said.
She has had pregnant women in the ICU too, their bellies swollen as a ventilator breathes for them.
And, in Colorado, just like the rest of the U.S., COVID-19 has been much harder on people of color.
Stay home now, don’t travel for Thanksgiving to honor and support nurses
To help all of the people who could get COVID-19, Olivia won’t be gathering with others outside of her home this Thanksgiving. She’s pleading with all other Coloradans to do the same. Experts at the Centers for Disease Control and Prevention are advising Americans not to travel this Thanksgiving and to only gather with people in their household.
“I know it breaks my husband’s heart,” Olivia said. “His family lives 15 minutes away. But, if we all get together, there will be 13 of us. This is just one year. If we can skip this one year, that means we can have many Thanksgivings in the future.
“Please skip Thanksgiving (with people outside of your home) this one year. Celebrate in the spring instead,” Olivia said. “Stay home. Stay safe.”
Olivia and her team will keep caring for those who need it. But, she worries that if infections keep rising at a record clip, they might not be able to keep up.
“We’re exhausted,’’ she said. “And, if we keep going, are we going to be able to take care of everyone?’’
After working well over 12 hours each day, Olivia tries to relax on the weekends with her husband and their boys. One of the boys’ favorite activities these days in taking all the cushions off the couch, lining them up end-to-end on the stairs, then racing down on old pieces of cardboard. They call them their “box slides.”
“I’m tired, but we find ways to have fun and unwind,” Olivia said.
When the boys ask why their mom is so busy, she gives them a simple answer.
“I just tell them that there are a lot of sick patients and right now, the coronavirus is getting bad again because people aren’t wearing their masks and being careful. That helps the boys do the right thing.”
