
A University of Colorado School of Medicine research team’s work on Alzheimer’s disease is yielding laboratory insights into the roots of the degenerative brain disease that have leapt to human clinical trials at UCHealth in short order.
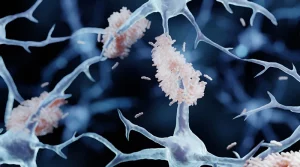
Their approach is to understand the biochemistry behind the development of Alzheimer’s disease plaques and the mechanisms of the cognitive decline it causes, find already-approved drugs that target those mechanisms, and demonstrate in studies with mice and then people that these therapies can be effective.

The team, led by neuroscientist Huntington Potter, professor of neurology at the University of Colorado School of Medicine and director of the CU Alzheimer’s and Cognition Center, has long had a focus on a long-since U.S. Food and Drug Administration (FDA)-approved drug called sargramostim (trade name Leukine), a synthetic version of granulocyte-macrophage colony stimulating factor (GM-CSF).
GM-CSF is a cytokine the body produces to stimulate aspects of the immune system. Potter’s research team has shown that the drug sargramostim, typically used as a bone-marrow stimulant to help patients recover from chemotherapy, also helps cognitive performance among mice genetically engineered to have Alzheimer’s disease – as well as among Alzheimer’s patients.
Alzheimer’s-Down syndrome connection
That work continues. A recent study led by Mahiuddin Ahmed, a PhD researcher in Potter’s lab, found sargramostim to reverse learning and memory deficits, the loss of certain nerve cells, and other brain abnormalities of mice engineered to have Down syndrome. The drug also showed cognition to improve in normal aging mice.
The Down syndrome connection is poignant: Those with Down syndrome have a vastly increased risk of Alzheimer’s disease over time, with 30% of those in their 50s and half of those in their 60s dealing with Alzheimer’s dementia. By age 40, the brains of nearly all of those with Down Syndrome have significant amyloid beta plaques and tau tangles, autopsies have shown.
It’s no accident, then, that Potter is also the director of Alzheimer’s disease and research at the Linda Crnic Institute for Down Syndrome at the Anschutz Medical Campus. It’s also no accident that Potter and colleagues recent research has focused on something that the above numbers make clear – plaques and tau tangles alone do not appear lead inexorably to Alzheimer’s disease. There’s something about particular plaques and tangles that cause problems.
Ahmed and colleagues’ sargramostim study helped land a National Institutes of Health (NIH)/National Institute on Aging grant to study sargramostim treatment in young adults with Down syndrome. The clinical study (a phase 2 clinical trial in FDA parlance), is set to launch at the UCHealth Neurology Clinic – Central Park, with CU School of Medicine and UCHealth neurologist Dr. Peter Pressman taking the clinical lead. That’s in addition to another phase 2 study Pressman is guiding at the Central Park clinic, Potter says. That one, currently recruiting patients, will study 42 people with mild to moderate Alzheimer’s disease, with 28 receiving sargramostim and 14 getting a placebo for 24 weeks.
The KIF11 gene
Other work by Potter and colleagues has led to insights as to what might cause certain amyloid beta plaques to cause Alzheimer’s and others seemingly to remain benign. A study by Esteban Lucero, a PhD researcher mentored by Potter and his CU Department of Neurology colleage Heidi Chial, PhD, found that the overexpression of a gene tied to cell division and the structure and function of neurons may protect against cognitive decline in both mice and humans in Alzheimer’s disease – even when amyloid beta is present.

The work built on studies Potter’s team did more than a decade ago that considered proteins that move other proteins to neurotransmitter and neurotrophin receptors in nerve cells. They found that inhibiting a gene called Kinesin-5 (also called KIFF11) blocked important functions in neurons. Lucero’s work took the opposite tack by asking what happens if you amp up, rather than suppress, KIF11.
The answer appears to be that nerve cells in petri dishes and in the brains of Alzheimer’s mice perform better despite the presence of amyloid beta plaques in the mice.
“Overexpressing KIF11 in mice did not affect the amyloid levels in the brain, yet they were still cognitively normal,” Potter said. “This is one of the best indications that you can maintain cognition without getting rid of the plaques.”
For a sense of KIF11’s effect on people with Alzheimer’s disease, Lucero and colleagues took an additional step of combing through data from the Religious Orders Study and the Rush Memory and Aging Project at Rush University in Chicago. They found that those with higher naturally occurring levels of KIF11 had better cognitive performance than normal among older adults with amyloid beta plaques. Potter says the team has gone on to compile a list of existing drugs (if they already exist, one can avoid the fearsomely expensive and time-consuming process of getting FDA approval for a new drug) and has submitted a grant to the NIH to investigate those drugs more thoroughly. A clinical trial of the best of them would then follow, Potter says.
An antidepressant and an antipsychotic
Along those same lines, Potter’s colleague and PhD neuroscientist Noah Johnson went hunting for existing drugs that block the effect of apolipoprotein E4 (APOE4). The gene that encodes the protein is, as Potter put it, “probably the strongest risk factor for Alzheimer’s disease other than age itself.” APOE4 promotes the formation of amyloid beta from amyloid beta peptide – the former being dangerous to the brain even as its precursor appears to be benign. Johnson and coauthors screened 595 compounds in an NIH drug library, identifying several that blocked the effect of APOE4 on Alzheimer’s amyloid beta formation.
 They then looked at the National Alzheimer’s Coordinating Center database to see what happened when someone was prescribed the drugs for normal indications but also had Alzheimer’s disease. They found that those receiving the antidepressant imipramine and antipsychotic olanzapine had improved cognition and diagnoses – and also that those two drugs, unique among other antidepressants and antipsychotics the team screened, inhibited APOE4’s creation of amyloid beta.
They then looked at the National Alzheimer’s Coordinating Center database to see what happened when someone was prescribed the drugs for normal indications but also had Alzheimer’s disease. They found that those receiving the antidepressant imipramine and antipsychotic olanzapine had improved cognition and diagnoses – and also that those two drugs, unique among other antidepressants and antipsychotics the team screened, inhibited APOE4’s creation of amyloid beta.
The next step is to test imipramine, which has fewer side effects than olanzapine, on a mouse model, after which a clinical trial on Alzheimer’s patients could follow, Potter says.
“The number of human drugs that have shown any benefit to Alzheimer’s disease patients are maybe one or two or three,” Potter said. “So this is a very promising advance.”
While the work of Potter’s team is diverse, “it’s all one complex but interrelated story,” he says.
To crack the many codes of a disease that affects some 6 million people and their families in the United States alone, “different approaches have to keep coming from open-minded scientists here and around the world,” Potter said.
